
The Importance of Preventative Measures to Public Health
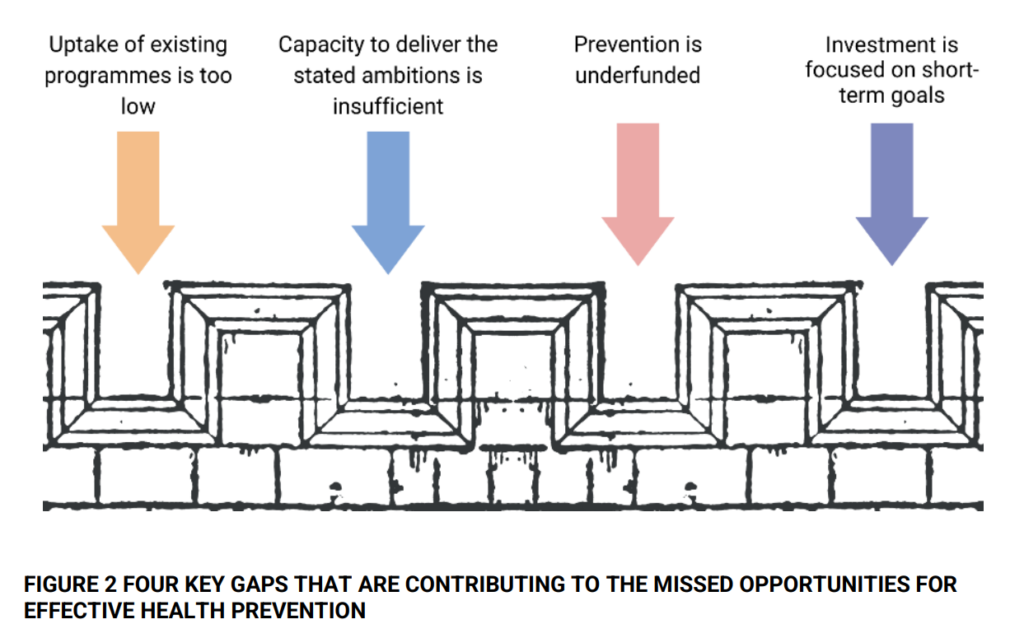
Both the government of the United Kingdom and the National Health Service (NHS) recognise the significance of prevention work within the medical field. Despite widespread knowledge, people often ignore beneficial preventative strategies. The public health grant has seen a cut of more than a quarter, or 26%, per person since the 2015/2016 fiscal year. This grant covers the delivery of public health services, including preventive measures. The cut has affected its real value.
Prevention is an investment of public resources that can lower the burden of ill health, strengthen the capacity of the health system, and support economic growth. Prevention is an extremely cost-effective investment. This term refers to the activities one performs to lower the chances of contracting a disease or illness. There are three categories of preventative measures:
- Primary prevention involves encouraging health before disease develops (for example, through vaccinations);
- Secondary prevention involves recognising disease at an early stage (through screening programs);
- Tertiary prevention involves reversing, stopping, or delaying the progression of disease (through chronic disease management programs).
The prevention of poor health is the responsibility of each and every government department, particularly in areas such as the environment, employment, income, education, and crime. Nevertheless, the focus of this paper is on preventative measures that can be taken within the context of the health sector in the UK.
Not only are prevention programs useful for people’s health, but they are also excellent for the economy. According to the findings of a comprehensive analysis, these programs have a return-on-investment ratio of 14 to 1 on average. As a result, budget cuts represent lost chances for the NHS to make savings in terms of both money and capability.
The Economic Impact of Prevention
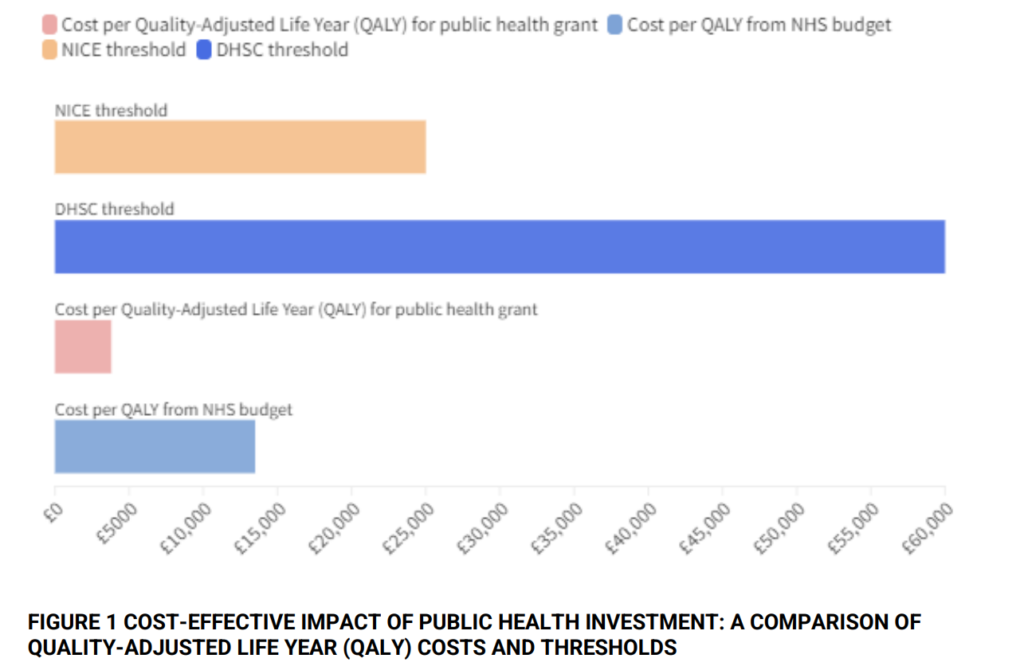
Preventative measures can lead to significant cost savings. It is expected to cost £3,800 for an additional year of good health through prevention. In contrast, treatment would cost £13,500 for the same period. Moreover, reducing preventable illnesses could potentially increase tax revenue. It could also decrease welfare payments and save costs for the police and criminal justice system.
Preventable illnesses cause the UK economy to lose over £70 billion annually due to lost productivity. A new era of prevention could come if we overcome the obstacles in the way. This could happen through long-term collaboration across parties, innovative financing, and using new opportunities. These opportunities include precision medicine and digital health.
Stakeholders can make substantial progress towards healthcare prevention goals by taking appropriate actions. Politicians should highlight the social benefits of prevention. The government, health authorities, and partner groups need to devise and execute prevention programs. Integrated care systems should prioritise prevention to benefit local communities and healthcare systems. Healthcare practitioners should prioritise disease prevention within their roles. The industry must innovate more in prevention and focus more on cost-efficient research and therapies. Economists and researchers should broaden the existing information pool and create new tools to facilitate change. The general population must take personal health responsibility to ensure the healthcare system’s sustainability.
In conclusion, making an investment in preventive can lead to huge rewards, both for one’s health and one’s wallet. It is time for us to shift our attention in the healthcare industry from decision-making and implementation in the short term to decision-making and implementation in the long term.
