
The Rising Challenge of Telehealth and CGM Technology in Diabetes Management
As we celebrate World Diabetes Day, we must acknowledge the growing burden of diabetes care. With 37.3 million people in the United States diagnosed with diabetes, the healthcare industry faces a tremendous issue. The number of endocrinologists, or diabetes specialists, is frighteningly low, with a patient-to-endocrinologist ratio of 1:4375. Because of this imbalance, the majority of diabetes care is now provided in primary care settings. However, resources and expertise may be restricted in these settings. Telehealth and Continuous Glucose Monitoring CGM technology in diabetes management might enhance care for these patients in a significant way.
Continuous Glucose Monitoring (CGM) Technology’s Potential
CGM technology has demonstrated promising improvements in managing both type 1 and type 2 diabetes. CGM can lower haemoglobin A1c levels, enhance time in range (TIR) of 70 to 180 mg/dL, reduce the occurrence of hypoglycemia, and improve quality of life. Despite these advantages, however, CGM adoption is not prevalent, particularly in primary care settings.
The VDiSC (Virtual Diabetes Specialty Clinic)
The VDiSC, or virtual endocrinology clinic, was created to bridge the gap between an increasing number of diabetes patients and a limited number of endocrinologists. It employs telemedicine to deliver comprehensive diabetic treatment, facilitate CGM integration into diabetes self-management, and provide behavioral health support. This virtual model provides patients with type 1 and type 2 diabetes with access to specialised care without the need for actual travel, making it a more practical solution for individuals who live in rural places or have mobility concerns.
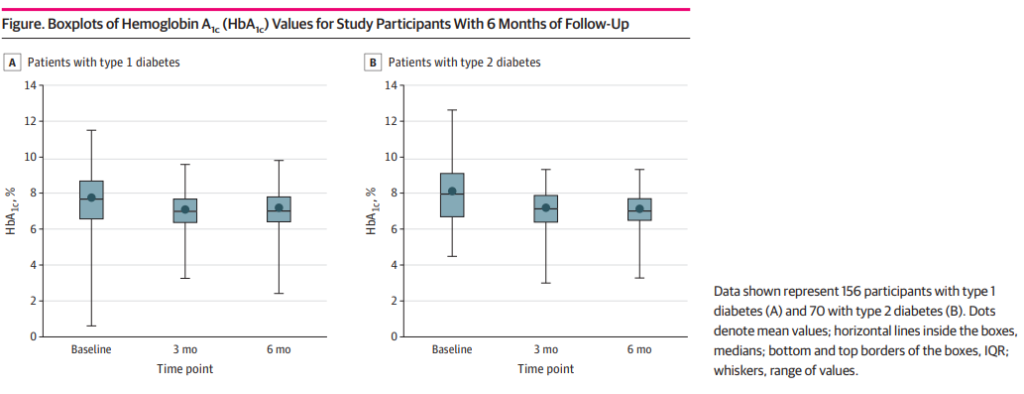
The JAMA study discovered that patients reported considerable benefits, including significant decreases in HbA1c levels and improvements in TIR. The VDiSC trial demonstrated that a virtual clinic care paradigm can deliver significant clinical advantages to diabetic patients. Telehealth services can potentially increase care access for everyone, reduce health inequities in communities, and aid in implementing breakthrough technology like CGM. The COVID-19 pandemic has made these services more accessible, showing promise for the management of chronic conditions like diabetes.
