Introduction
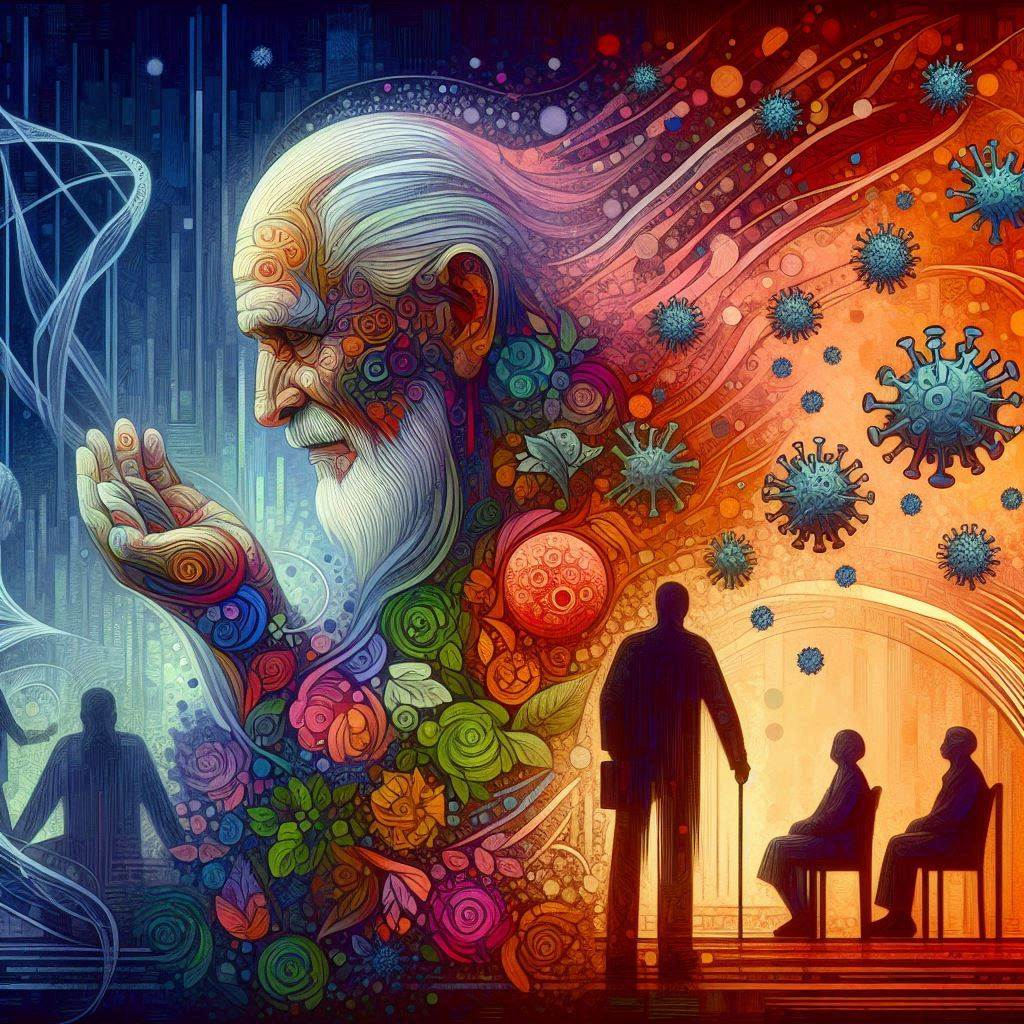
The interplay between infections and chronic health conditions is an important aspect influencing ageing and longevity, intricately linked to economic dynamics. The impact of immunosenescence on ageing is a critical area of study in the healthcare industry. Immunosenescence, which refers to the gradual deterioration of the immune system associated with ageing, plays a crucial role in shaping health outcomes. Inflammageing, which refers to the chronic pro-inflammatory state, also plays an important role in this process. This decline in immune system affects the body’s ability to fight infections and respond to vaccinations. Understanding this process is vital for developing strategies to improve health outcomes for the elderly.
Understanding Immunosenescence
Immunosenescence is characterised by a decline in the functionality of the innate immune system. This includes ineffective pathogen recognition and reduced macrophage activation. Studies show that by age 65, the thymus, which produces T-cells, has lost 60% of its original size. This reduction leads to a decreased diversity in the T-cell repertoire, making the elderly more susceptible to infections.
Chronic Inflammation and Ageing
Recent medical insights highlight the profound influence of individual infection history on health deficits and mortality risks. Chronic inflammation, or inflammageing, is closely linked to immunosenescence. As people age, they often develop a persistent pro-inflammatory state. Consequently, this condition can lead to various chronic diseases, including cardiovascular disease, type 2 diabetes, and Alzheimer’s disease. Furthermore, research indicates that inflammageing is a core mechanism associated with the ageing process.
Impact on Infectious Diseases
The impact of immunosenescence on infectious diseases is profound. Therefore, elderly individuals are more vulnerable to infections like influenza and pneumonia. The COVID-19 pandemic highlighted this vulnerability, with older adults experiencing higher mortality rates. A cytokine storm, a severe immune reaction, can lead to organ failure and death in these individuals.
Modelling Infectious and Chronic Diseases
A recent model developed by Strulik and Grossmann explores the interplay between infectious and chronic diseases. It investigates how health deficits accumulate and affect survival probabilities in detail. Individuals make decisions on consumption, disease prevention, health investments, and savings, subject to budget constraints. The model maximises expected lifetime utility, considering factors like interest rates, mortality rates, and income. It explores how individuals allocate resources to optimise utility over their lifetimes, factoring in the impact of infectious diseases on chronic conditions. The calibration of the model for a typical American man in 2010 highlights the complex relationship between health behaviours, economic factors, and disease prevention strategies. The model provides insights into how individuals make choices regarding protection against diseases, considering factors like age, health status, and economic circumstances.
Strategies for Mitigation
Addressing the impact of immunosenescence on ageing requires a multifaceted approach. The proposed model integrates the interaction between infectious and chronic diseases into the economics of aging, highlighting the role of immunosenescence and inflammation. This approach demonstrates how a history of infections accelerates the development of chronic health deficits, influencing disease severity and mortality with age. By incorporating health spending decisions, the model points out the importance of early and continuous protection against infections to mitigate long-term health impacts. Thus, enhancing vaccination efficacy in the elderly is crucial. Moreover, promoting healthy lifestyles can mitigate chronic inflammation. Research into therapeutic interventions targeting immunosenescence is ongoing, offering hope for improved health outcomes.
Conclusion
Insights into the economic underpinnings of ageing and health outcomes offer a nuanced understanding of the intricate relationship between infections, chronic conditions, and socioeconomic factors. Addressing the decline in immune function among the elderly can enhance their life expectancy and quality of life while also reducing the burden of infectious diseases. Therefore, this study integrates biological mechanisms with economic frameworks to offer a holistic view of the factors influencing health trajectories and longevity trends. Through this approach, valuable insights are provided into the complex dynamics of healthcare economics and ageing.
