
Introduction
Optimising communication between patients and clinical teams is crucial in improving the quality of care and patient satisfaction, particularly following a cancer diagnosis. Patient-reported outcomes (PROs) have emerged as a key facilitator of this communication, revealing symptom patterns that clinicians might overlook. Remote patient monitoring (RPM), a digital innovation, enables patients to report PROs electronically (ePROs), allowing healthcare teams to monitor symptoms and intervene in real-time. A recent publication explored the real-world implementation of remote patient monitoring in oncology and RPM across 33 centres in Europe, focusing on its impact on patient engagement and symptom management.
Remote Patient Monitoring in Oncology
PROs provide a direct insight into the patient’s experience, particularly in terms of symptom incidence and trajectories. Studies have consistently shown that integrating PROs and ePROs into oncology care enhances communication, reduces symptom burden, improves quality of life, and boosts treatment adherence. The European Society of Medical Oncology (ESMO) has recognised these benefits, recommending the implementation of RPM systems that connect patients and healthcare teams with proactive alerts for severe symptoms.
Despite the proven advantages, the adoption of ePROs in routine clinical practice faces several challenges. These include provider resistance, data accuracy concerns, privacy issues, reimbursement hurdles, and technological illiteracy. The COVID-19 pandemic, however, accelerated the introduction of RPM systems in oncology due to the increased need for decentralised care. Large multicentric initiatives, especially in North America, have demonstrated RPM’s feasibility but highlighted the need for optimised clinical pathways and digital systems to achieve optimal participation and clinical impact.
Implementation of RPM Pathway in Europe
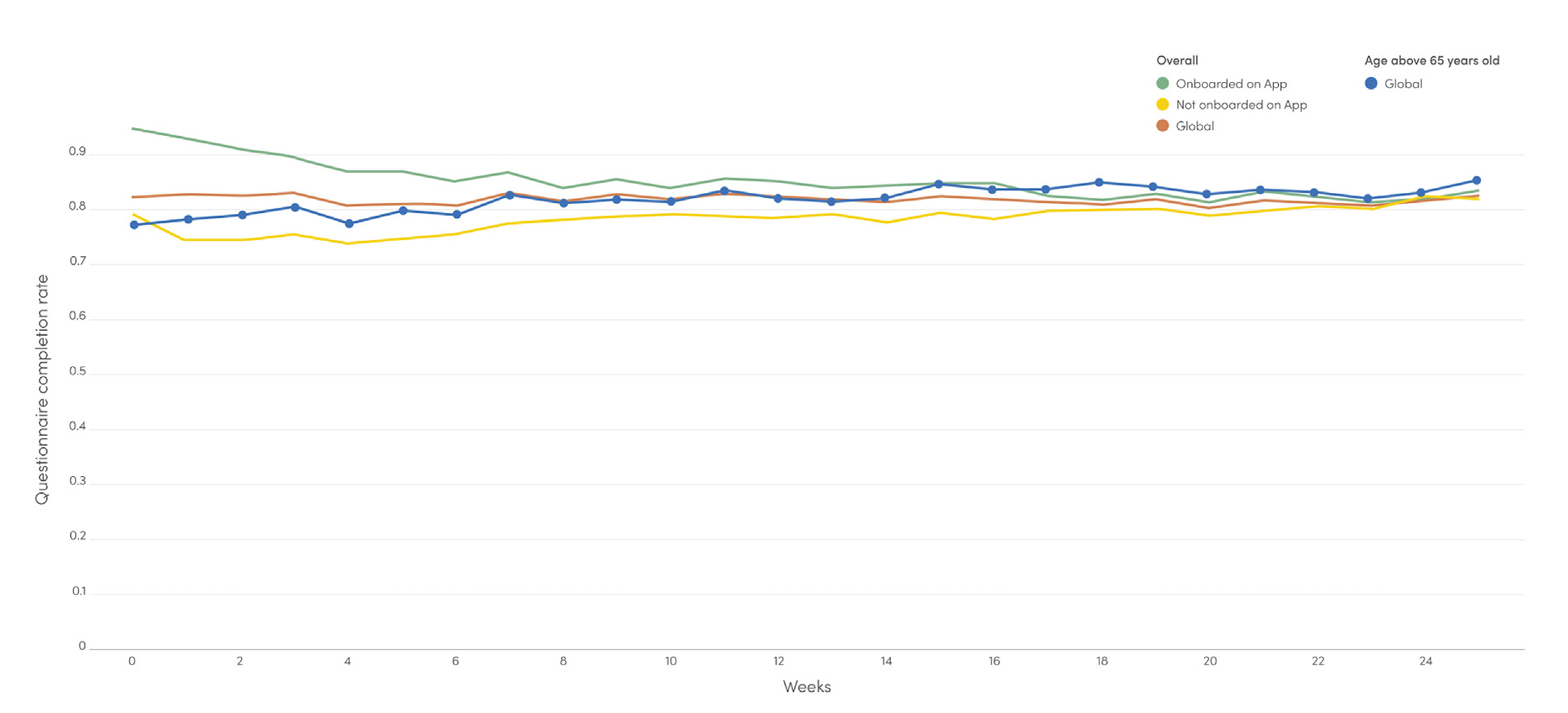
The study reports on the implementation of an RPM pathway across 33 centres in France and Belgium, enrolling 3015 patients from November 2021 to August 2023. The pathway demonstrated high patient engagement, with an average compliance rate of 82% for weekly ePROs. Nurse navigators responded to patients’ alerts within a median time of 13 hours and 41 minutes, leading to significant reductions in symptom severity.
Several factors contributed to the high level of patient engagement observed in this study. A structured and well-defined implementation process, adaptive to various barriers, played a crucial role. This process considered software functionality, measured outcomes, personnel deployment, leadership, culture, workflow, and patient engagement. The study also benefited from prior experiences and guidelines, such as the CAPRI trial and recommendations from the PROTEUS Consortium.
The RPM pathway was co-designed with input from healthcare professionals (HCPs), researchers, patients, and technology experts. Patient representatives were involved in all phases of development, ensuring that the technology met their needs. The RPM technology solution, Resilience PRO, included features that enhanced patient engagement and empowerment, such as a library of educational content personalised to the patient’s symptoms.
Challenges and Future Directions
Despite the success, challenges remain in implementing RPM in routine care. These include the need for organisational changes within cancer care centres, such as dedicated teams for RPM planning, deployment, patient onboarding, and alert management. The recent announcement by the French Ministry of Health to reimburse RPM for chronic conditions, including cancer, is expected to accelerate adoption by addressing financial and structural obstacles.
In the United States, the Centers for Medicare & Medicaid Services (CMS) has reimbursed remote therapeutic monitoring (RTM) since late 2022, following specific criteria. The inclusion of a chat functionality in the Resilience PRO platform in pilot centres since August 2023 aims to further improve alert management and reduce HCP burden.
Conclusion
The real-world implementation of an RPM pathway across 33 cancer centres in France and Belgium has proven feasible and effective, with high levels of patient and provider engagement. The RPM pathway facilitated significant improvements in symptom control, demonstrating its potential to enhance oncology care. Future studies will focus on evaluating the impact of educational content, optimising alert management, and assessing cost-effectiveness.
