
Introduction
Psoriasis, a chronic inflammatory skin condition affecting working-age individuals, primarily manifests as psoriasis vulgaris, constituting over 80% of cases. Psoriasis treatment and healthcare resource utilisation (HCRU) are critical topics in dermatology. Linked to various comorbidities like psoriatic arthritis and cardiovascular diseases, psoriasis imposes a substantial healthcare burden, particularly in Europe where it affects 1-5% of the population. Biologics targeting immune pathways have significantly advanced treatment, yet real-world data on HCRU patterns remain scarce.
Understanding Psoriasis Burden and Comorbidities
A retrospective study from Finland provided a comprehensive analysis of the real-world impact of biologic treatments on HCRU in psoriasis patients. In Finland, psoriasis treatment aligns with Current Care Guidelines, reserving biologics for severe cases unresponsive to initial therapies. The study analysed data from Finnish national health registers, focusing on patients who initiated biologic or conventional treatments between January 2013 and December 2017. The biologics included in the study were adalimumab, brodalumab, etanercept, secukinumab, ixekizumab, certolizumab pegol, and ustekinumab, as they are reimbursable for psoriasis treatment in Finland. Conventional treatments included cyclosporine, methotrexate, and acitretin. Biologic initiators, predominantly male, exhibited higher rates of immune-mediated comorbidities compared to conventional starters.
Key Findings
Reduction in Dermatology Visits
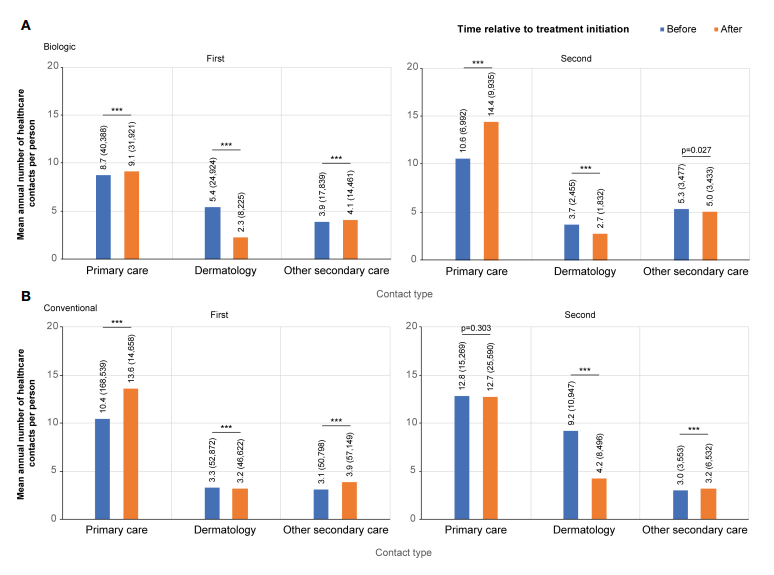
One of the most significant findings was the reduction in dermatology visits among biologic starters. The mean annual number of dermatologist contacts decreased from 5.4 to 2.3 per person after initiating biologic treatment. This reduction highlights the effectiveness of biologics in managing psoriasis, leading to fewer healthcare visits.
Impact on Primary and Secondary Care
While dermatology visits decreased, the mean annual number of primary care and other secondary care contacts slightly increased after starting biologics. Primary care contacts rose from 8.7 to 9.1 per person, and secondary care contacts increased from 3.9 to 4.1. These findings suggest that while biologics reduce the need for specialised dermatology care, they may lead to increased interactions with less costly healthcare providers.
Treatment Switching
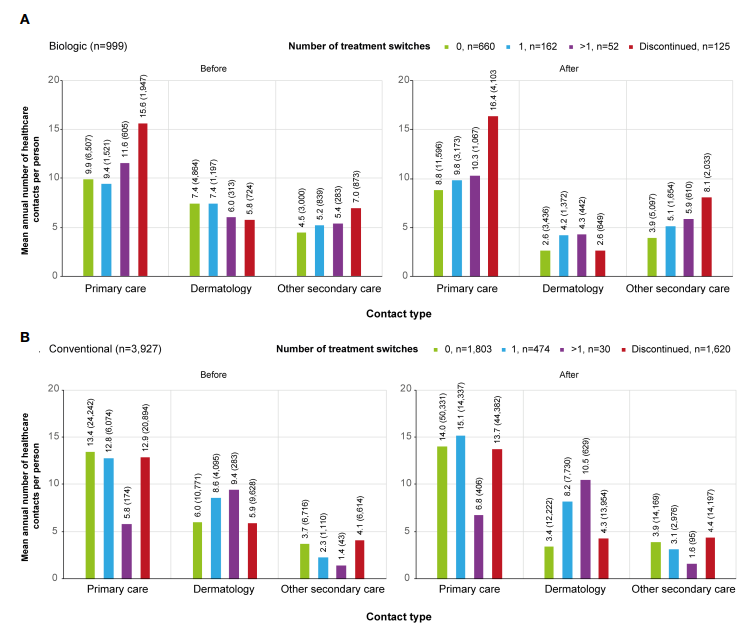
Switching treatments, common in both groups, influenced HCRU differently. Approximately 32.3% of biologic starters and 19% of conventional starters switched treatments at least once during the observation period. Biologic switchers experienced milder peaks in dermatologist visits, indicating smoother transitions. Conversely, conventional switchers exhibited heightened dermatologist contacts pre-switch, suggesting unmet treatment needs. Notably, non-switching biologic users demonstrated lower overall HCRU compared to switchers, implying treatment continuity’s positive impact.
Limitations and Considerations
The study had several limitations, including a lack of detailed clinical information and the exclusion of private and occupational healthcare data. Besides, the analysis did not include drugs administered in hospitals, such as intravenous infliximab. Despite these limitations, the study provides valuable insights into the real-world impact of biologics on HCRU in psoriasis patients.
Conclusion
This study demonstrates the benefits of biologic treatments in reducing dermatology visits and highlights the importance of considering patient needs and preferences in psoriasis management. As the number of treatment options continues to grow, understanding the real-world impact of these treatments becomes increasingly important. The findings support the use of biologics to improve patient outcomes and reduce the burden on healthcare systems.
