Patient-Reported Outcomes Measures (PROMs) have emerged as a pivotal tool in healthcare. Healthcare settings have applied PROMs in numerous instances since the advent of Value-Based Care (VBC), gaining valuable insights into patients’ perceptions of their health and treatment outcomes.
PROMs in VBC
According to the FDA, PROMs are “reports coming directly from patients about how they feel or function in relation to a health condition and its therapy, without interpretation by healthcare professionals or anyone else.” Essentially, the definition emphasizes patient-centred care, where patients’ experiences and outcomes are central to healthcare delivery.
However, this begs the question: Are the current methods of capturing PROMs sufficient, or can we leverage today’s advanced technologies to optimise this process? The answer lies in the potential of artificial intelligence (AI) and electronic Patient-Reported Outcomes (ePROs).
Enhancing PROMs with AI and ePROs
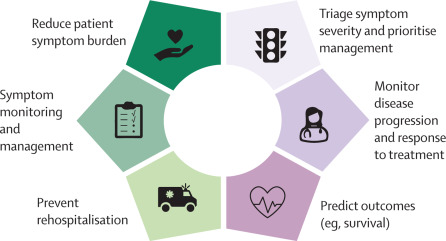
Integrating PROs can significantly improve the patient journey, from symptom screening to treatment planning. This approach enables continuous feedback, providing real-time evidence of outcomes without the need for numerous follow-ups. The dynamic nature of this process also improves the perceived value of the cost per episode (CPE) for the patient.
AI tools can augment this area further by providing tailored support based on the severity of illness, eliminating the inefficiencies and frustrations caused by inappropriate care levels. For instance, an oncology trial in 2016 utilised a web-based symptom reporting system to automatically alert clinicians about reported symptoms. The system, although not AI-based, proved cost-effective, improved patient survival, reduced emergency visits, and enhanced the quality of life (QoL).
The Future of PROMs in Healthcare
NICE stated that evaluation of such solutions is necessary in the future. However, one must not lose sight of the patient’s perspective amidst the rush towards a digital space.
Previous articles discussed the risk of these solutions lacking a patient-centred approach and provided other “moonshot” solutions to address this. The lack of patient or person-centred care dehumanises the care continuum which poses a risk to VBC.
The potential of a PRO model lies in its dual approach: as an input into an AI model predicting an outcome, and as an output from an AI model predicting changes in symptoms or QoL. This captures the lived experience of the patient. In a pilot study, the system demonstrated its ability to predict the likelihood of patients achieving Minimal Important Clinical Difference (MCID). This was after a Total Knee Arthroplasty (TKA).
However, the design’s fragmented nature and lack of representation of the diverse population it serves remain significant challenges. Biases in AI and validated system training limitations can skew the model. This could perpetuate many of the inherent issues.
To mitigate these challenges, it’s recommended that PROs become standard practice, prioritised, and incorporate the patient experience as a key metric. Careful consideration must be given to PROMs integration. The focus must be user-centred to ensure ease of use and optimised workflows. International guidelines such as The Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) highlight elements of good design.
The inclusion of these systems has the potential to improve health and QoL by supporting better and faster patient-centred care. To ensure clinician utilization and patient integration, we need to take several steps. These steps will help in achieving a high-value outlook. Patient-Reported Outcomes Measures, augmented by these tools, can significantly influence healthcare system navigation, optimising the continuum of care, and improving outcomes.
