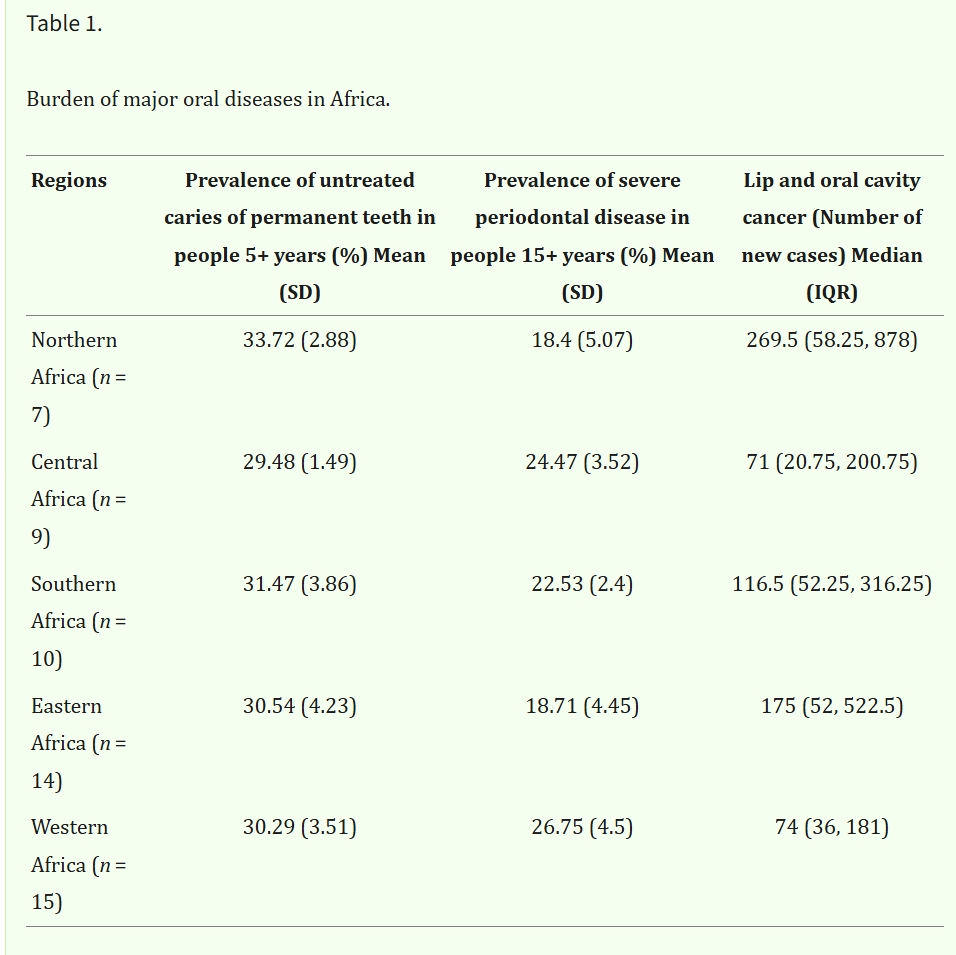
- Oral Disease Burden: Untreated dental caries and periodontal disease are widespread in Africa. Regional variations are influenced by socioeconomic and dietary factors.
- Workforce and Policy Gaps: Many countries face a critical shortage of dentists and dental care assistants. Inadequate oral health policies worsen the problem.
- Collaborative Solutions: Partnerships among healthcare providers, industry, civil society, and academia are key to improving oral health outcomes.
- Prevalence of Oral disease: Untreated caries (5+ years) is highest in Northern Africa (33.72%), severe periodontal disease (15+ years) in Western Africa (26.75%), and new lip and oral cavity cancer cases in Northern Africa (median: 269.5 cases). See Table 1 for details.
Background Context:
WHO reports Africa has seen the largest global rise in oral diseases over 30 years. Nearly 44% of the population is affected. Only 57% of African countries have a national oral health policy. The region spends less than US$1 per person annually on oral health. WHO’s Global Oral Health Strategy aims for universal coverage by 2030, focusing on prevention and community-based interventions.
Implications:
- Health Economics: Oral diseases cause significant economic losses due to healthcare costs and lost productivity. Prevention and better care access can bring long-term benefits.
- Health Outcomes: Integrating oral health into primary healthcare and community interventions can improve overall well-being.
- Policy and Research: Strengthening local research is vital for evidence-based policies.
To address these issues effectively, stakeholders must take coordinated action. In particular, integrating oral health into national public health policies remains essential for expanding access to care. Furthermore, national dental associations, working in partnership with public health institutions and international organisations, can drive meaningful policy change and promote better resource allocation. Through such collaborative efforts, Africa can begin to close the oral health gap and deliver improved outcomes for its population. For more details, see the original article.
