
Introduction
Life expectancy (LE) improvements have reshaped demographics globally, particularly in high-income countries, where individuals are living longer. However, the focus is shifting towards not just longevity but also healthy ageing. Health-adjusted life expectancy (HALE) plays an important role in assessing overall population health, reflecting the balance between lifespan and quality of life. As populations in industrialised countries age, healthcare systems face significant challenges. Understanding the healthcare system responses to ageing populations, disease burden among older adults, and the dynamics between life expectancy, HALE, and healthcare performance is crucial for shaping effective healthcare strategies for the ageing population.
Increasing Life Expectancy and Health-Adjusted Life Expectancy
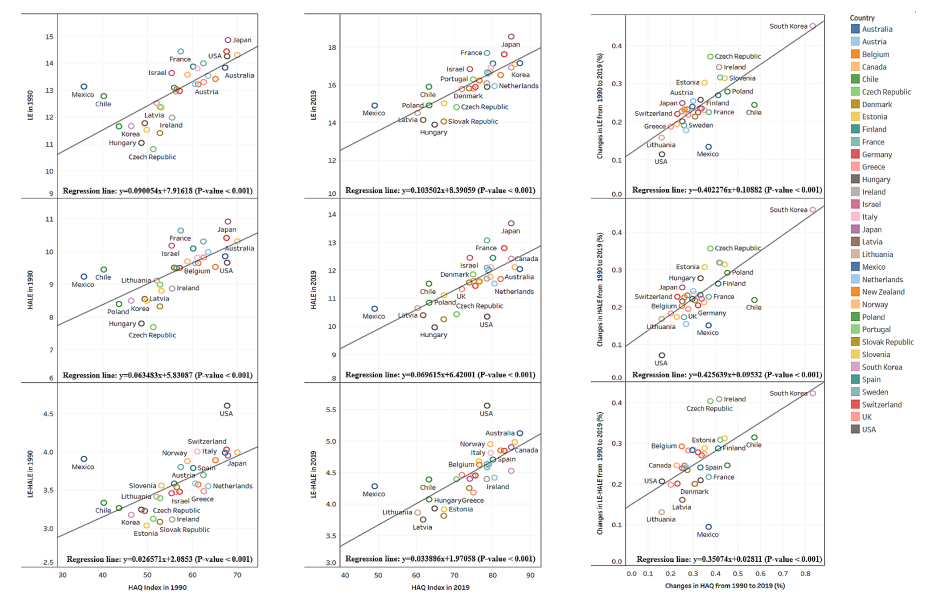
In a comprehensive study across 33 industrialised nations, significant increases in both LE and HALE among individuals aged 70-74 were observed from 1990 to 2019. The Global Burden of Disease Study 2019 (GBD 2019) provides comprehensive data on these trends. For individuals aged 70 and above, LE and HALE have shown notable improvements. These advancements were closely linked to improvements in Healthcare Access and Quality (HAQ) indices. HAQ index, introduced by GBD 2019, helps assess whether health systems provide quality care across different regions. The study found that an improved HAQ index correlates with increased LE and HALE. However, the rise in unhealthy years of life (LE-HALE), measured by years lived with disability (YLD) and disability-adjusted life years (DALY), raises concerns about the sustained burden of morbidity among older adults.
The Burden of Disease Among Older Adults
The GBD 2019 data reveals that non-communicable diseases (NCDs) are the primary contributors to the disease burden among older adults. These include cardiovascular diseases, cancers, and chronic respiratory diseases. The study categorises diseases into four levels, with NCDs being a significant concern at Level 1.
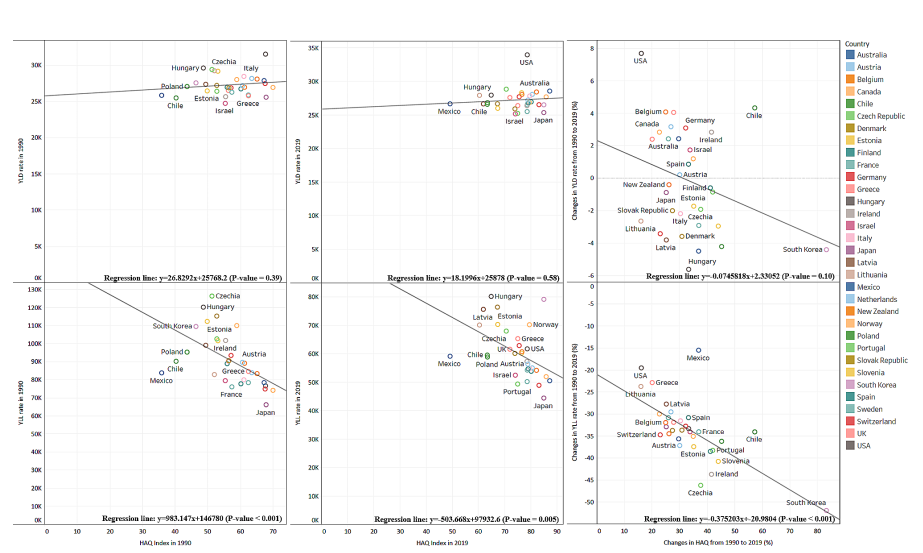
Years of life lost (YLL) due to premature mortality have decreased with a higher HAQ index. However, the changes in YLD are relatively small and not significantly correlated with the HAQ index. This indicates that while people are living longer, they are also spending more years in poor health.
Healthcare System Challenges
Healthcare systems in high-income countries must adapt to the increasing morbidity burden among older adults. The rising number of unhealthy years of life suggests a need for better management of chronic diseases. In 2019, Latvia, Lithuania, and Mexico showed significant increases in YLD, highlighting the need for targeted healthcare interventions.
The economic and social implications of an ageing population are substantial. Healthcare needs and expenditures are expected to rise, placing a considerable burden on healthcare systems. For instance, in South Korea, chronic diseases accounted for 85% of total medical costs in 2022. This highlights the importance of focusing on reducing morbidity and disability caused by chronic diseases.
Addressing Challenges and Looking Ahead
As populations age rapidly in high-income countries, healthcare systems must adapt to the changing demographics and health profiles of their populations. The findings emphasise the importance of reorganising healthcare systems to provide age-friendly services that effectively manage chronic conditions and promote healthy ageing. Efforts towards combating ageism, fostering age-friendly environments, integrating care services for the complex needs of elderly, and ensuring equitable access to quality healthcare services for all age groups are essential points for promoting healthy ageing in the coming years.
Conclusion
The increasing LE and HELA in industrialised countries are positive trends, signalling improved healthcare outcomes. However, the concurrent rise in unhealthy years of life necessitates a re-evaluation of healthcare strategies to mitigate the burden of morbidity among older populations. By fostering age-friendly healthcare systems and implementing tailored public health initiatives, we can strive towards healthier and more fulfilling ageing experiences for all.
