Introduction
Pneumonia, a major cause of childhood mortality, claims more than 700,000 young lives annually, with a significant burden in regions like sub-Saharan Africa and South-East Asia. While the pneumococcal conjugate vaccine (PCV) has proven effective, its adoption worldwide varies, particularly in lower-middle-income countries (LMICs). Due to the high cost of PCV, these countries struggle to integrate it into their immunisation programs. Strategic pricing policies are crucial for achieving global immunisation goals, alleviating disparities in pneumonia vaccine access and obtaining equitable vaccine affordability for all nations.
Current Disparities in Pneumonia Vaccine Access
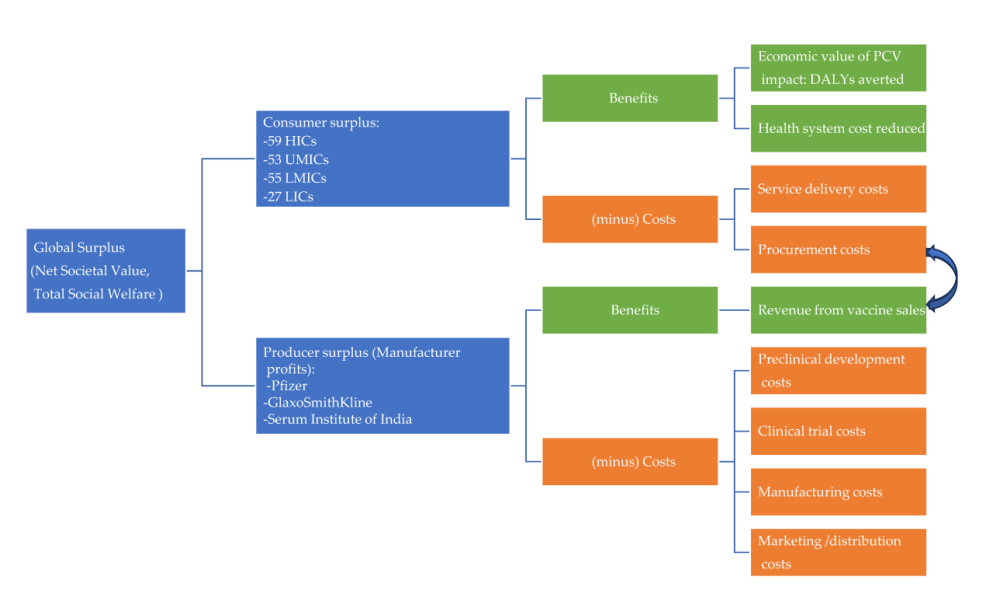
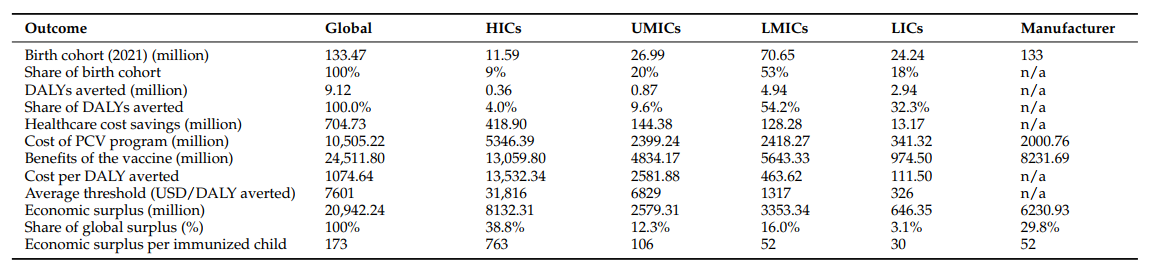
In 2021, the World Bank classified 194 countries and territories into distinct income categories, including high-income countries (HICs), upper-middle-income countries (UMICs), lower-middle-income countries (LMICs), and low-income countries (LICs). The consumer benefits of PCV are determined by calculating the monetized value of health advantages, like avoiding disability-adjusted life years (DALYs), and cost savings from reduced disease burden in healthcare.
At present, HICs and manufacturers predominantly benefit from PCV’s economic surplus, whereas LMICs receive less than 6% of the total global surplus. Innovative pricing approaches are essential to ensure broader access to PCV, especially in regions with high disease burdens. Efforts such as tiered pricing and clinical trials for optimised dosing aim to enhance affordability and accessibility. However, challenges persist, with some countries facing escalating vaccine costs and delayed access to new, life-saving vaccines.
Promoting Equitable Vaccine Access
To mitigate disparities, regional cooperation, cross-subsidisation strategies and alternative procurement strategies, can drive down vaccine costs and enhance accessibility of vaccines in LICs. Pooled procurement allows countries to combine purchasing power, leading to significant savings and an increased economic surplus. For example, a pooled procurement partnership established in 2012 among Estonia, Lithuania, and Latvia led to a price reduction ranging from 17% to 25% per immunisation course. Pooled procurement mechanisms also achieved 42% lower prices than self-procurement for 18 widely used vaccines in MICs in 2022. Notably, the recent availability of lower-priced vaccines like Pneumosil® has shown promise in increasing affordability for LMICs. Promoting equitable vaccine access can indeed lead to wider adoption and improved health outcomes.
Future Directions
While progress has been made in reducing vaccine prices and expanding access, ongoing efforts are needed to ensure equitable distribution of vaccine benefits. As new manufacturers enter the market and patents expire, further price reductions are anticipated, potentially enhancing global vaccine access.
In addition, achieving the World Health Organization’s (WHO) Immunization Agenda 2030 (IA2030) target of 90% vaccination coverage would significantly increase the global economic surplus. The total surplus would rise from USD 15.9 billion to USD 20.9 billion. However, the distribution remains skewed, with HICs and manufacturers still receiving over 68% of the surplus. This indicates that simply increasing coverage does not address the uneven distribution of vaccine benefits.
Conclusion
In conclusion, current vaccine pricing policies disproportionately benefit HICs and manufacturers, who receive the highest share of the economic surplus generated by PCV. Unaffordable prices, limited health budgets, and lack of transparency in price setting hinder vaccine uptake in MICs. Early adoption of pooled procurement mechanisms, promoting vaccine manufacturing in LMICs, and implementing more steeply tiered prices could enhance vaccine access globally. These insights provide a foundation for developing future pricing policies and ensuring broader access to vital vaccines for all communities.
