
Introduction
Financial protection in healthcare is crucial for ensuring that households do not face undue financial hardship due to medical expenses. This concept is a cornerstone of Universal Health Coverage (UHC) and is emphasised by Sustainable Development Goal 3.8.2, which aims to reduce catastrophic healthcare expenditure (CHE). However, many low- and middle-income countries struggle to provide affordable, high-quality healthcare, primarily due to out-of-pocket (OOP) payments. This issue is particularly pronounced in India, where a significant portion of healthcare costs is borne directly by households.
The Burden of Out-of-Pocket Payments
In India, approximately 65% of healthcare expenses are incurred through OOP payments, making it one of the highest globally. This financial burden leads to catastrophic healthcare expenditure for 49% of Indian households seeking medical care, pushing 15% into poverty. The older population is especially vulnerable, with over half affected by chronic health conditions (CHC) and a quarter suffering from multi-morbidity.
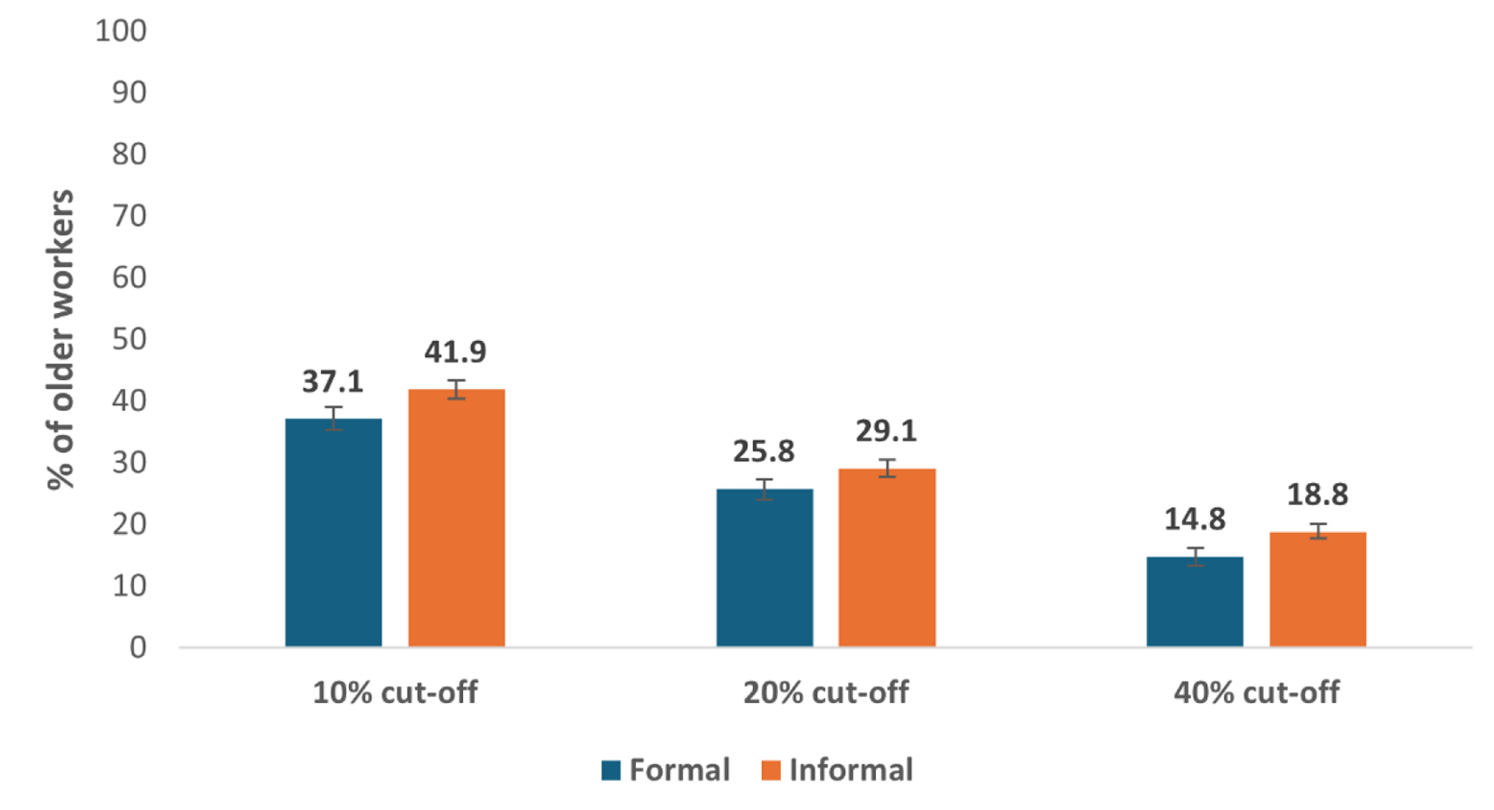
Medicines are the primary contributor to OOP payments, accounting for about 70% of total healthcare costs. The reliance on private healthcare and the lack of adequate medical and social insurance exacerbate the financial strain on households. Despite this, government health expenditure remains low, at just 1.15% of the gross domestic product (GDP). In the informal sector, 18.8% spend more than 40% of their income on healthcare expenditure (Figure 1).
Informal Sector and Healthcare Challenges
India’s labour market is predominantly informal, with around 92.4% of the workforce engaged in informal employment. These workers lack secure employment contracts, social protection, and worker benefits. As a result, many older individuals continue to work past the retirement age of 60 years due to financial necessity.
Previous research indicates that continuing to work into old age is a survival strategy in countries with inadequate social safety nets. In India, approximately 33 million people work beyond retirement age, primarily in the informal sector. These workers face significant challenges in accessing healthcare due to their lower wages and lack of financial protection.
Government Initiatives and Their Shortcomings
Several initiatives have been launched to provide financial aid to informal workers, such as the Janashree Bima Yojana and the Universal Health Insurance Scheme. However, these programs have faced numerous implementation challenges. The Unorganised Workers Social Security Act also fell short of providing adequate social security.
The Rastriya Swasthya Bima Yojana (RSBY) aimed to address these shortcomings but encountered similar issues. The Ayushman Bharat Program (ABP), launched to enhance healthcare accessibility and affordability, has also faced significant challenges, including corruption and insufficient participation.
The Way Forward: Policy Recommendations
To address the healthcare challenges faced by older informal workers, several policy recommendations can be made.
- Enhancing insurance coverage is crucial. Expanding health insurance coverage to include a broader segment of the older population, particularly those in the informal sector, can help reduce the burden of OOP payments and provide financial protection.
- Improving public healthcare facilities is another key step. Investing in high-quality, subsidised public healthcare facilities can improve accessibility and reduce the reliance on private healthcare providers.
- Raising awareness about available healthcare programs and the rights of informal workers is essential. Information and communication technology can be used to disseminate this information effectively.
- Strengthening social security systems is vital. Developing robust social security systems that provide financial and healthcare protection for informal workers is necessary. This includes ensuring timely and adequate benefits and addressing issues such as corruption and irregular payments.
- Regular monitoring and evaluation of healthcare policies and programs are necessary to ensure they meet their objectives and provide the intended benefits.
Conclusion
India faces significant challenges in providing financial protection and healthcare access to its older informal workers. Addressing these issues requires a multifaceted approach, including enhancing insurance coverage, improving public healthcare facilities, raising awareness, and strengthening social security systems. By implementing these recommendations, India can better protect its older population from financial hardship and improve their overall health and well-being.
