
A recent article from Zorginstituut Nederland reports that elderly care costs in 2025 are expected to rise significantly in the Netherlands. The announcement highlights the increasing financial pressures on the Dutch health system. Demographic shifts and greater demand for complex, long-term care are primary drivers of these budgetary increases. This forecast anticipates substantial expenditure growth for sectors vulnerable to aging and chronic conditions. Ongoing governmental discussions about financing and ensuring sustainable access continue.
Key Drivers of Increased Care Expenditure
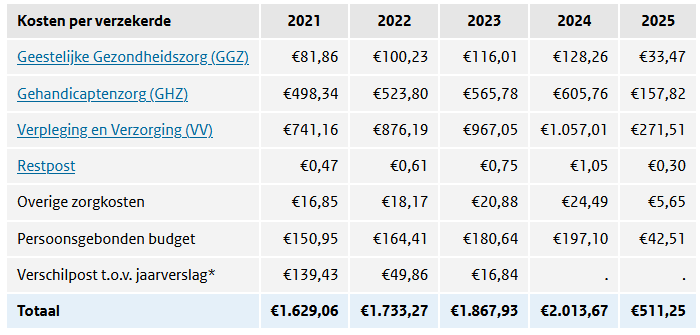
The increasing expenditure is driven by the interplay of demographic changes, notably an aging population, and heightened needs for specialized care services. These factors drive costs in the long-term care sector and GGZ. Projections for 2025 indicate higher utilization of nursing homes, home care, and outpatient mental health support. The report further notes persistent staff shortages exacerbating operational costs, along with ongoing post-pandemic challenges affecting mental health service demands. Policymakers expect that per-capita spending will increase in alignment with the growing population of elderly and chronically ill citizens. Moreover, the complexity of multimorbidity means that more resource-intense care delivery is required. These trends illustrate the challenges facing policymakers in balancing fiscal sustainability with access and quality care.
Global Health Economics Context
To contextualize these Dutch findings within the broader health economics landscape, it is beneficial to consider similar global dynamics. Health systems worldwide are grappling with budget constraints, workforce shortages, and increased demand for complex, personalized care. This mirrors the situation in the Netherlands. The international and Dutch contexts reinforce the necessity to adapt financing mechanisms and delivery models to respond to new demographic and clinical realities.
The projected rise in elderly care costs in 2025 for Dutch services has broad implications for reimbursement decisions, and long-term system sustainability. Policymakers and payers are likely to experience increased pressure to emphasize value-based care initiatives. They will also conduct more rigorous health technology assessments to maximize return on investment. The scaling of long-term and mental health care may require new risk-sharing arrangements with providers and innovative payment models.
Demand is escalating for home-based and community-integrated services—a trend observed in both European and North American markets. Lastly, these developments are expected to drive advancements in digital transformation and workforce optimization. Stakeholders seek improved productivity amid persistent labor shortages and fiscal constraints. In conclusion, the Dutch experience reflects the converging pressures present across high-income health systems. It highlights the urgent need for adaptive policy frameworks and cross-sector collaboration to ensure access and affordability in an evolving healthcare landscape.
For more detailed insights into the projected costs and implications for elderly care in 2025, you can read the full report from Zorginstituut Nederland here.
