
Introduction
Psoriasis is a chronic skin condition affecting millions worldwide. Due to its visible manifestations, psoriasis often subjects patients to stigma and discrimination, significantly impacting their social and psychological well-being. The economic burden is also substantial, with costs related to treatment and lost productivity. Despite advancements in treatment, significant gaps in psoriasis care persist. A recent in-depth analysis examines these gaps and explores how health systems can better meet patients’ needs. By addressing these issues, it is possible to improve the quality of life for those living with psoriasis.
Epidemiology of Psoriasis
The prevalence of psoriasis varies significantly across different regions. Estimates of the total disease burden also vary significantly, ranging from about 40.8 million to 60 million people globally, according to the Global Burden of Disease (GBD) data and the Global Psoriasis Atlas (GPA). For instance, in France, estimates vary from 1-2% to nearly 5% of the population. In contrast, Asian countries like China and Japan report lower prevalence rates of 0.21% and 0.34%, respectively.
The incidence is higher among lighter-skinned individuals and older people. However, misdiagnosis is a concern among darker-skinned individuals and children. In high-income countries, the age-standardised incidence is almost double the global average, at 112.6 per 100,000 compared to the global average of 57.8 per 100,000.
Current Care Environment
Current methods of psoriasis treatment include topical creams for mild cases, oral systemic medications and injectable biologics for moderate to severe cases, often used in combination. Due to the systemic nature of the disease and high likelihood of comorbidities, its treatment often necessitates the involvement of specialists such as dermatologists and rheumatologists. However, access to these specialists varies widely, as the referral pathway is often convoluted, leading to delays in diagnosis and treatment. Patients frequently face long waiting times and the burden of navigating a fragmented healthcare system.
Despite high response rates, many patients find these treatments burdensome, particularly due to the high costs of newer therapies and feelings of dissatisfaction. Consequently, many do not receive the continuous, comprehensive care needed, resulting in suboptimal outcomes and a diminished quality of life.
Societal and Economic Burden of Psoriasis
The burden of psoriasis extends beyond skin manifestations, with up to 30% of patients estimated to struggle with psoriatic arthritis. Mental health issues related with psoriasis also play an important part, with depressive symptoms affecting 28% of patients and a heightened risk of suicidal ideation, particularly among younger individuals with severe disease manifestations.
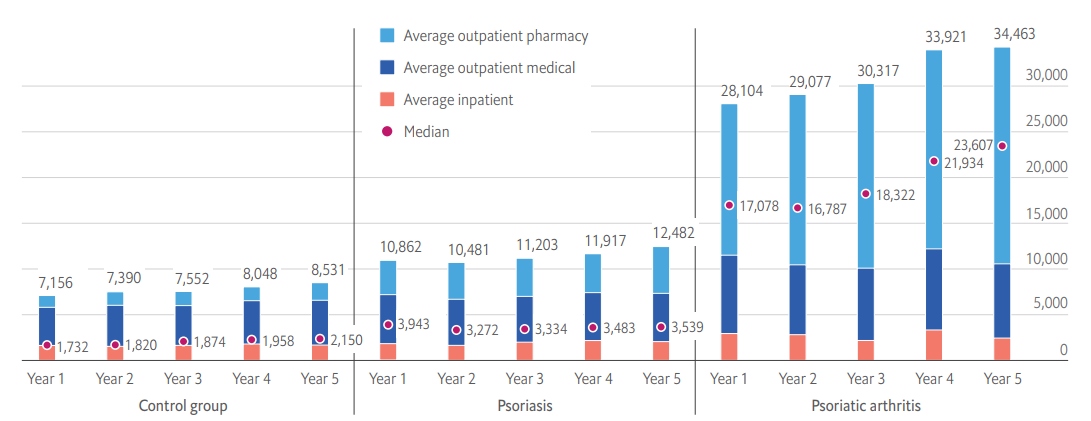
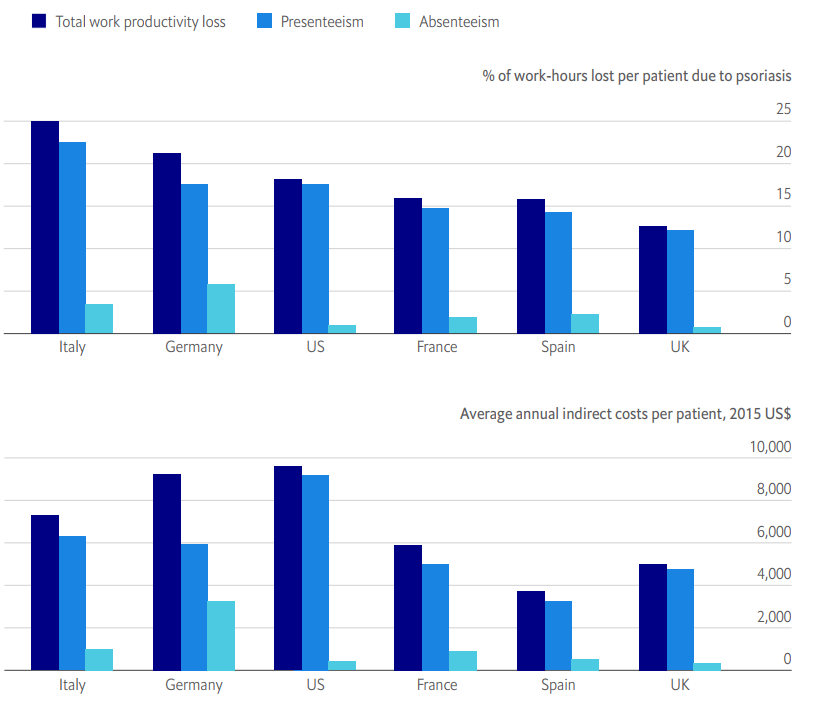
The direct health costs of psoriasis are staggering, with a US study finding that all-cause healthcare costs for psoriasis patients in the first year of treatment average US$10,862. These costs nearly triple to US$28,104 for patients affected by psoriatic arthritis. Moreover, the annual indirect costs per patient due to work productivity losses range from US$3,742 in Spain to US$9,591 in the US.
Identifying Gaps in Psoriasis Care
Several gaps in psoriasis care have been identified. These include delays in diagnosis, limited access to specialists such as dermatologists, and inadequate treatment options. Furthermore, there is a lack of comprehensive care that addresses both physical and psychological aspects of the disease. Health systems often fail to provide continuous support, leaving patients to navigate their care journey alone.
Opportunities for Improvement
To bridge these gaps, several strategies can be implemented. Increasing public awareness and education about psoriasis is essential. This can reduce stigma and encourage early diagnosis. By enhancing healthcare provider education, prioritising patient-centred care, providing equitable access to care through telemedicine, and advocating for patient empowerment and shared decision-making can also make a significant difference in patients’ quality of life. Furthermore, integrating psychological support into treatment plans can improve overall patient well-being.
