Introduction
Chronic obstructive pulmonary disease (COPD) is a prevalent lung condition characterised by airflow obstruction and breathing difficulties. Long-term exposure to air pollution, tobacco smoking, and genetic factors are recognised as primary risk factors for COPD. This disease significantly affects sufferers’ health-related quality of life (QoL), often measured by utility values on a scale from 0 (death) to 1 (perfect health). Understanding these utility values is crucial for evaluating the cost-effectiveness of various interventions. A recent study aimed to update a meta-analysis from 2015 to determine whether there have been changes in mean utility values for COPD.
The Importance of Utility Values in COPD
Utility values play a pivotal role in health economics, particularly in cost-utility analyses. These values are used to calculate quality-adjusted life-years (QALYs), which help health policymakers assess the cost-effectiveness of medical interventions. The National Institute for Health and Care Excellence (NICE) prefers using utilities derived from the generic EuroQol 5 Dimension (EQ-5D) instrument for consistency in health economic analyses. However, significant variability in utility values across different studies poses a challenge to ensuring consistency in these analyses.
EQ-5D Utility Values in Adults with COPD
The recent meta-analysis included 65 studies that reported EQ-5D based utility values for adults with COPD. After rigorous screening, 42 studies were included, yielding 104 data points for analysis. The studies spanned various regions, with a notable number of data points collected in Asia. The most common method of elicitation was EQ-5D-3L. The average age of study participants was 66.6 years, with 64.94% being male. The mean FEV1% predicted was 54.5%, indicating moderate airflow obstruction.
The meta-analysis revealed several key findings:
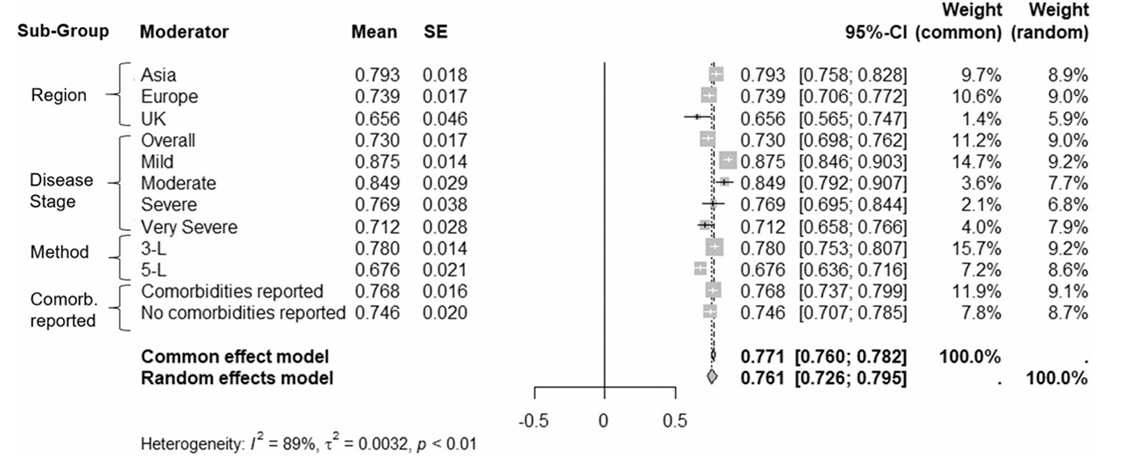
Variability in Utility Values: Significant heterogeneity was observed in utility values among COPD patients. This variability demonstrates the need for a systematic approach in selecting the most relevant utility values for cost-utility analyses.
Impact of Disease Stage: The study found that utility values decreased with increasing disease severity. The mean utility values for mild, moderate, severe, and very severe stages were 0.875, 0.849, 0.769, and 0.712, respectively.
Regional Differences: Studies conducted in the UK reported a mean utility value of 0.656, while those in Asia reported a higher mean utility value of 0.793. This significant difference suggests that regional factors may influence health-related QoL.
Method of Elicitation: The EQ-5D-5L measurement tool yielded a lower mean utility value (0.676) compared to EQ-5D-3L (0.780). The increased sensitivity of EQ-5D-5L allows for a more nuanced capture of health impacts.
Comorbidities: Reporting of comorbidities did not significantly impact the meta-analysed mean utilities. However, the consistency in reporting comorbidities across studies is crucial for future research on their impact on QoL.
Implications for Future Research and Practice
The findings highlight the importance of considering various factors when selecting utility values for health economic models. Researchers and policymakers should systematically examine the method of elicitation, disease stage, and regional differences. The results from this meta-analysis can inform future cost-utility analyses, ensuring more accurate and generalisable findings. Moreover, the increased awareness and better adherence to treatment plans, early detection, and advancements in medical treatments have likely contributed to the improved health-related QoL of COPD patients.
Conclusion
The recent meta-analysis provides valuable insights into the variability and factors influencing COPD utility values. Understanding these factors is crucial for evaluating the cost-effectiveness of interventions and improving the quality of life for COPD patients. Researchers and policymakers must continue to refine their approaches to ensure accurate and consistent utility values in health economic analyses.
