
Introduction
Diabetes mellitus, a chronic condition affecting millions globally, demands nuanced decision-making across various aspects of patient care. Effective management hinges on informed choices regarding medication, diet, lifestyle, and treatment options. Multicriteria Decision-Making (MCDM) techniques offer a systematic approach to navigate the complexities of diabetes care.
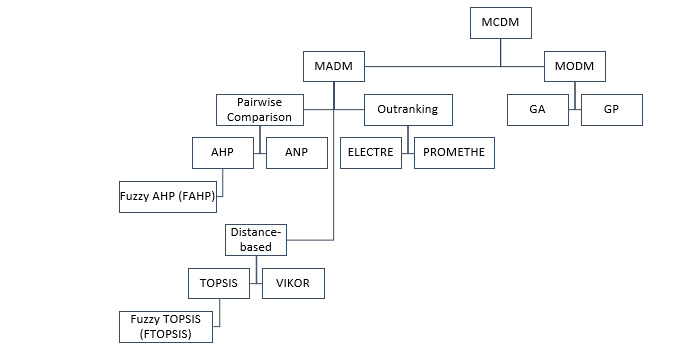
By analysing 63 articles from 2003 to 2023 using the PRISMA method, distinct categories emerged, including medication selection, diagnosis, meal recommendations, management, complications, and prevalence estimation. Notably, the Analytic Hierarchy Process (AHP) emerged as a prominent tool across these categories, offering structured decision-making support. The findings underscore the versatility and potential impact of MCDM techniques in optimising diabetes care.
Medication Selection
Among the key areas where MCDM techniques shine is in medication selection. Studies reveal that MCDM methods, particularly AHP, play a pivotal role in aiding clinicians in choosing optimal diabetes medications. By weighing factors like efficacy, safety, and cost, these techniques facilitate evidence-based decisions tailored to individual patient needs.
Diagnosis and Meal Recommendations
MCDM techniques extend beyond medication selection, encompassing diagnosis and meal planning. From predicting diabetes risks to recommending dietary choices, these methods provide structured frameworks for healthcare providers to navigate the complexities of diabetes care. Notably, AHP emerges as a versatile tool in guiding diagnostic decisions and meal recommendations for patients with diabetes.
Diabetes Management and Complications
Effective diabetes management requires a comprehensive approach that considers various factors such as social support, treatment compliance, and risk assessment for complications. MCDM techniques, including ANP and TOPSIS, aid in assessing current mHealth applications, prioritising resources, and evaluating the severity of diabetes-related complications. These methods offer a holistic view of diabetes care, enhancing decision-making processes for healthcare providers.
Future Research
The integration of MCDM techniques in diabetes management proves instrumental in optimising patient care and treatment outcomes. By offering structured decision-making frameworks, these methods empower healthcare providers to make informed choices across various aspects of diabetes care. As the prevalence of diabetes continues to rise, leveraging MCDM techniques can significantly enhance the quality of care provided to individuals with diabetes, ultimately improving health outcomes and quality of life.
Future research should explore integrating MCDM techniques with AI and machine learning to enhance decision-making in diabetes care. Tailoring MCDM methods to individual patient needs can promote personalised medicine. Expanding MCDM applications to areas like mental health assessment and long-term disease management is recommended. Involving a broader range of stakeholders will ensure user-friendly tools that meet diverse needs. Optimising resource allocation using MCDM methods can improve healthcare efficiency and access. Clinical trials and real-world evidence are needed to validate MCDM effectiveness.
