
Introduction:
Cervical cancer, a leading cause of cancer-related deaths among women worldwide, is predominantly caused by persistent infection with high-risk human papillomavirus (HPV) types. The burden is disproportionately higher in low- and middle-income countries (LMICs) due to limited access to preventative measures and screening facilities. In 2020, over 80% of new cervical cancer cases occurred in these regions.
The HPV Vaccine and Its Global Importance:
The World Health Organization (WHO) introduced vaccines against HPV infection in 2006 and has recommended them since 2009. These vaccines form a key element of the WHO’s Global Strategy to Accelerate Cervical Cancer Elimination. The strategy sets a target to fully vaccinate 90% of girls against HPV by age 15 by 2030. However, the implementation cost presents a major concern for LMICs. The primary reason is the delivery of the HPV vaccine in school-based settings, which reduces opportunities for economies of scope.
The Economic Burden of HPV Vaccination:
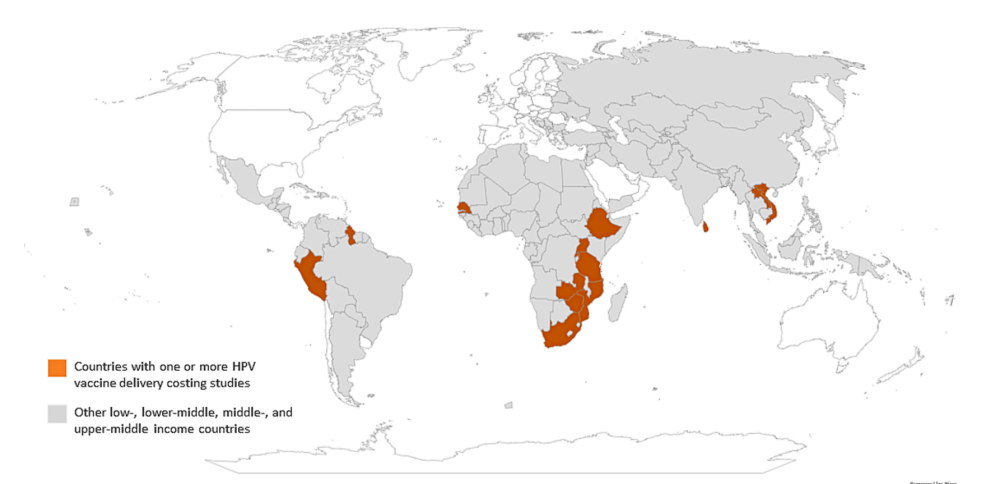
A systematic review published in 2022 focused on the programmatic costs and cost-effectiveness of HPV vaccination in all income settings. However, the included studies collected cost data during a program’s demonstration, pilot, or introduction phase, and empirical evidence from established national HPV vaccination programs was lacking. A recent study, however, summarises 15 empirical studies from 14 countries on HPV vaccination delivery costs. The cost per dose, excluding vaccine and supplies, ranged from $0.31 to $24.07, while the economic cost per dose ranged from $1.48 to $48.70 in 2022 US$. The economic cost per dose, which takes into account both direct and indirect costs, ranged from $1.48 to a staggering $48.70 in 2022 US$. This significant variance can be attributed to a multitude of factors, including the phase of implementation, geographical location, and delivery strategy.
Intricacies of HPV Vaccination Costs:
Interestingly, the review found no clear pattern in delivery costs across different phases of implementation. In some countries, such as Rwanda and Zimbabwe, HPV vaccine delivery costs per dose declined with time since introduction. However, in Uganda and Senegal, the cost per dose estimates modestly increased with program maturity. There was also substantial variation in costs across different geographies within the same country. These insights underline the complexity of HPV vaccination costs and highlight the need for further research to inform budgeting and financing priorities for HPV vaccine introduction and program sustainability.
Conclusion:
This systematic review presents an updated synthesis of the available evidence on the cost of HPV vaccination delivery in LMICs. The findings underscore the variability of delivery costs across and within countries and by phase of implementation. These insights are crucial for global healthcare strategies, particularly in the context of the ongoing fight against cervical cancer. However, the review also highlights significant gaps in current research, emphasising the need for more studies in countries outside of Africa, cost studies for single-dose schedules, strategies to improve coverage, and a more detailed exploration of in-country cost variations. A more comprehensive understanding of these factors is key to informing budgeting and financing priorities for HPV vaccine introduction and program sustainability, ultimately contributing to global efforts to eliminate cervical cancer.
