In the realm of healthcare, the concept of value-based care (VBC) is not new. Introduced by Michael Porter, VBC emphasises the importance of generating positive outcomes per unit of currency spent. Today, VBC is a driving force behind efforts to improve clinical outcomes while reducing costs. Central to this strategy is care management. This is designed to support selected patients via multidisciplinary teams to improve health-related outcomes.
The Role of Care Management in Value-Based Care
Care management programmes aim to assist with disease management, optimise care pathways through the healthcare system, and manage the utilisation of costs within the system. These programmes have encouraged participation by offering incentives, resulting in valuable data collection and improved efficiencies. However, despite these advances, patient-centred care is often overlooked in the current systems.
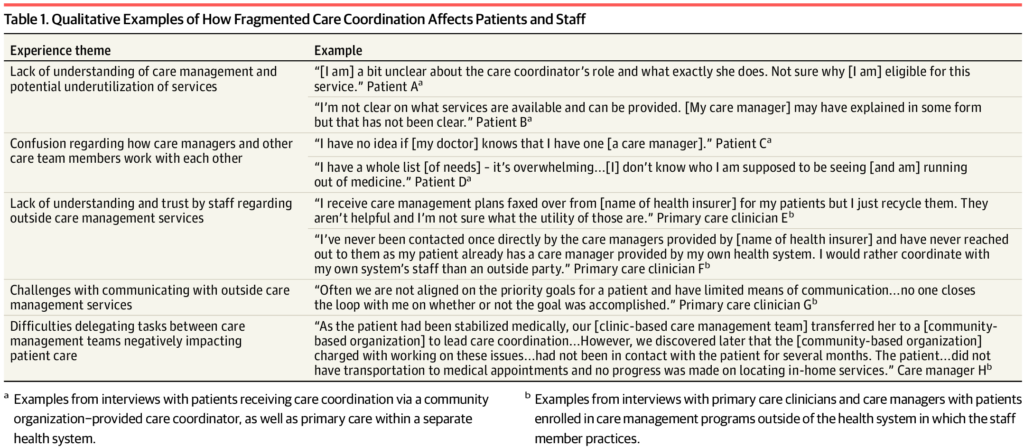
Understanding value in healthcare can be subjective. For some patients, value is about achieving personal health goals, even if these don’t translate into financial value for the health system. Fragmentation of care is also a notable challenge within these systems. It increases the complexity of patient care. With the entry of venture capitalists and other players into the healthcare system, effective care management has become essential for optimising performance and decreasing fragmentation.
A New Approach to Value-Based Care
The need for a patient-centred comprehensive care management continuum is becoming increasingly clear. This reframing of the VBC strategy consists of five key areas:
- Recognising that patients are multidimensional and their care trajectories fluctuate with their evolving health conditions;
- Offering a continuum of care management programming support matched to their specific needs;
- integrating and coordinating efforts to maximise resource utilisation;
- Committing to regular evaluation of broad program effectiveness;
- Redefining value from a person-centred and health equity-based perspective.
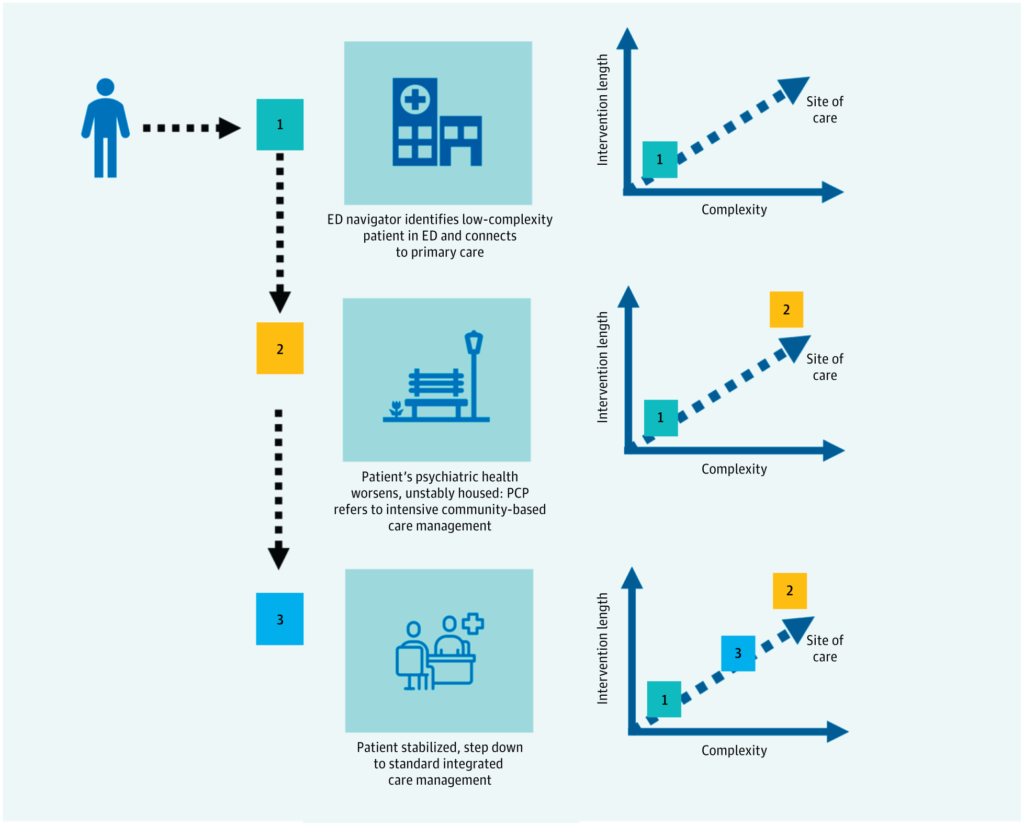
In line with the Just-In-Time (JIT) management philosophy, the concept of “the right program for the right patient” has emerged. This approach opens multiple access points for people to enter the system and offers various options for care. Patients are then graded to determine the level of care they need, from basic community health programmes to integrated care management for the most complex cases.
The Future of Care Management
Many innovation models require care management, and developers are creating alternative reimbursement models to promote comprehensive approaches. These models encourage care management for vulnerable populations and ensure rigorous evaluations by reviewing patient-centred outcomes. By introducing matrices for patient populations and attaching incentives, outcomes can improve.
Minimising the financial burden on patients and optimising the standard siloed approach to managed care are also key considerations. Multiple organisations can provide and coordinate care, but the proliferation of program offerings threatens to exacerbate the fragmentation of care delivery.
To promote patient-centred care management, health systems can benefit from providing a patient-tailored continuum of care management offerings. This would also provide an improved understanding of the care management ecosystem available to patients. Policymakers have a similar responsibility and opportunity to develop incentives to address worsening fragmentation in this field and to promote a more holistic, equitable, and patient-centred approach to care management aligned with value-based care.
As we move forward into the future of healthcare, the focus on value-based care and patient-centred care management will continue to shape the industry. The evolution of these concepts and their application in real-world settings will undoubtedly lead to improved patient outcomes and more efficient healthcare systems.
Image in text taken from the journal article linked below