The healthcare industry has faced significant challenges recently which has led to escalating costs. These have also continued to expand the disparities within healthcare worldwide. The COVID-19 pandemic brought these to light, with the marginalised communities experiencing higher rates of infection, morbidity, and mortality. These communities also continued to experience greater care disruptions. But what can be done about this? How could technology look to improve the outcomes and provide value? The quintuple framework proposes valuable aspects to improve healthcare systems and coupled with this, AI technologies can look to scale these improvements.
The Quintuple Aim
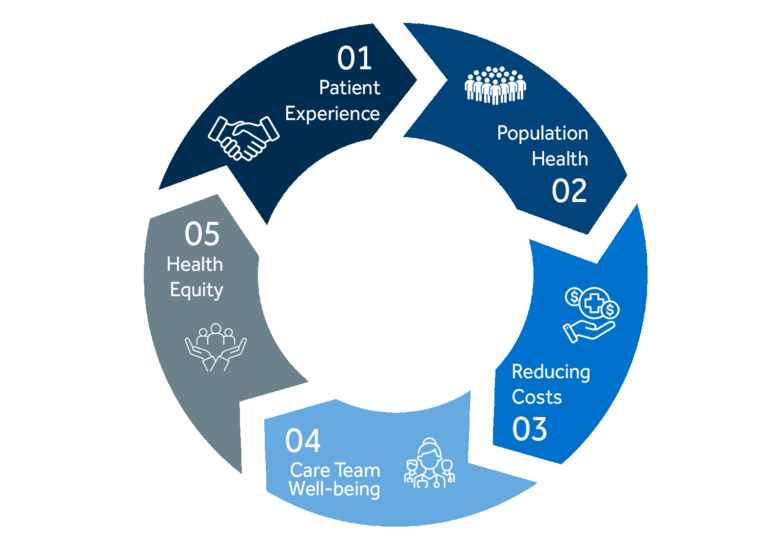
The need to optimise healthcare outcomes and reduce economic waste is more critical than ever. The triple aim was introduced as a beacon to guide healthcare improvements, focusing on enhancing population health, improving care experience, and promoting cost efficiency. However, the rising burnout rates among physicians and the increasing desire to leave the industry necessitated the inclusion of a fourth aim: addressing provider well-being. Without this, quality improvements would be unsustainable. The fifth aim was updated to include health equity, which ensures that we explicitly address equity and actively explore new efforts to promote it.
The quintuple aims for healthcare improvement are:
- Improving population health
- Enhancing care experience
- Cost Efficiency
- Provider Wellbeing
- Health Equity
The Role of Technology and Policy
Technology, particularly AI, plays a crucial role in achieving these aims. AI can improve access to equitable health, ensure cost-effectiveness through predictive algorithms, and manage procedural or administrative work through virtual assistants. Oracle Health has recently shown its new work in the healthcare space and optimising clinical models through the use of LMMs (multimodal models), by launching their digital assistant. The view is that it reduces the cognitive load on clinicians optimising the clinical delivery process, which ultimately also keeps it human. In turn, improvements to patient safety (increased clinician awareness), experience, and provider well-being are immediately actualised. These in turn allow for the other aims to occur as a direct outcome of these enhancements.
Policies based on these principles are essential for designing effective economic supports. Through explainable AI systems, value-based care incentives, and appropriate demographic data, outcomes can be improved, and care can be enhanced in any resource setting.
Cover image taken from: Chess Health Solutions
